![]()
In this episode, we are joined by Laura Legg, Director of Revenue Integrity Solutions at BESLER, to discuss the causes of mid-revenue cycle vulnerabilities and what hospitals can do to minimize risk and safeguard revenue.
Podcast (hfppodcast): Play in new window | Download
Learn how to listen to The Hospital Finance Podcast on your mobile device.Highlights of this episode include:
- Ways in which hospital revenue integrity departments are breaking down silos in healthcare revenue cycles.
- A look at the causes of coding vulnerabilities in the revenue cycle.
- What hospitals can do to minimize risk and safeguard revenue with coding and clinical documentation.
- Why hospitals should invest more in important resources such as people, processes and technology.
- And more…
To view the transcript of this podcast episode, click HERE
Tune in to our podcast episode “Exploring top revenue cycle issues” and learn what hospital leaders identified as their top 3 biggest revenue cycle challenges facing their hospitals today.
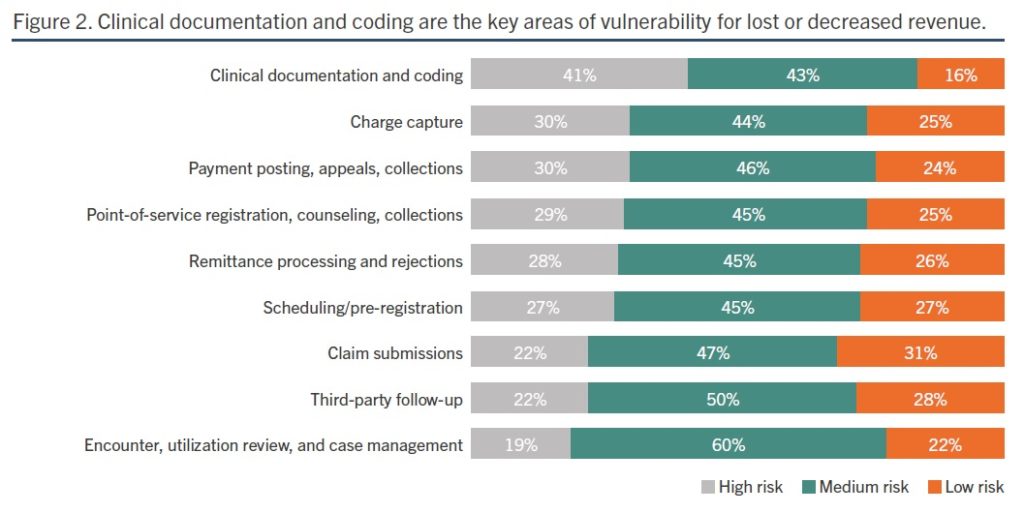
Clinical documentation and coding are perceived to be the most vulnerable areas of the revenue cycle
Recent HIMSS Media/BESLER research showed more than eight in 10 finance, revenue cycle, reimbursement and health information management leaders call clinical documentation and coding a high or medium risk area for lost or decreased revenue (Figure 2). This is often referred to as the mid-revenue cycle.
The ICD-10 coding system, used by Medicare and some insurance companies to determine a set lump-sum payment for hospitals to treat specific diagnoses, is constantly changing. That continual change makes it difficult for hospital staff to follow and comply. The ability to quickly and continuously train staff on ICD-coding updates is arduous.
Under ICD-10, coding accuracy scores for DRG assignment are much lower than they were under ICD-9.
In this episode, Laura Legg delves into the causes of mid-revenue cycle vulnerabilities and what hospitals can do to minimize risk and safeguard revenue.
Transcript for “Most vulnerable areas of the healthcare revenue cycle”
Mike Passanante: Hi, this is Mike Passanante. And welcome back to the Hospital Finance Podcast.
Recently, BESLER and HIMSS Media conducted a survey that looked at how to drive optimal revenue cycle performance. As part of that survey, we asked the respondents to tell us about areas that they saw as being most vulnerable in the revenue cycle.
And to shed some light on those findings and explain what we did find in the study, I’m joined by Laura Legg who is the Director of Revenue Integrity Solutions at BESLER.
Laura, welcome back to the podcast.
Laura Legg: Thank you Mike. And thanks for inviting me.
Mike: Laura, when we’re talking about vulnerable areas of the revenue cycle, what first comes to mind for you?
Laura: Well Mike, revenue cycle in healthcare is now such a complex system and supported by so many diverse activities. But sometimes, it’s really challenging for revenue cycle leaders to no longer think of revenue cycle as just finance.
Today’s healthcare revenue cycle is really an enterprise-wide responsibility with many stakeholders and team members working together. Breaking down isolated silos in those departments that work together can be challenging and was recently cited in the HIMMS Media study to identify the top hospital revenue challenges today.
The study included over a hundred respondents employed in leadership roles within finance, revenue cycle, reimbursement and HIM in US hospitals in acute care facilities.
Systems that are as complex as healthcare revenue cycle are likely to have vulnerabilities. Identifying those revenue cycle vulnerabilities is often done through a revenue integrity effort as long as department silos can be broken down.
Mike: Laura, do you think that revenue integrity departments are breaking down those silos in healthcare revenue cycle?
Laura: I do Mike. The same study shows that 47% of US hospitals now have revenue integrity departments. So that’s almost half. Bringing departments together, seeking common revenue integrity goals is working in those hospitals and having a positive impact on net revenue, reimbursement and decreasing denials.
There is still work to be done though, especially in those most vulnerable areas of revenue cycle.
Mike: So, let’s talk about the study results specifically. Laura, can you walk us through what respondents said were the most vulnerable areas of the revenue cycle?
Laura: I can Mike. And according to the study as well as some respondents I had on a recent Besler-sponsored webinar, they all overwhelmingly agree that the most vulnerable areas of the revenue cycle are coding and clinical documentation, often referred to as the mid-revenue cycle.
Accurate clinical documentation is the foundation of a legal medical record and billing encoding. It’s also the most complex and vulnerable part of the revenue cycle because independent providers must document according to sometimes vague payer rules.
It’s often difficult to hold physicians and other documenters accountable for applying the rules if they’re not well-educated.
So, any hospital’s plan in Medicaid vulnerability has to include physician and clinical staff training.
CDI should be working with providers for concurrent documentation audit and correction. HIM then comes in, reviews the documentation at discharge for completion, and then code the record to the optimal DRG assignment.
If all the previous steps in the revenue cycle have occurred correctly, then coders should have all the elements they need for coding. There should be very few physician query from HIM coders if coding is clearly supported through documentation.
Getting all of this right while the patient is still in the hospital will facilitate accurate coding and produce a clean claim to avoid backend correction and later denied payments.
Mike: So Laura, you’ve got a lot of experience in coding. You’re an expert in it. What do you think are the causes of that vulnerability in coding specifically?
Laura: Well Mike, there are a couple. One of the reasons for vulnerability in coding is the complexity of the ICD-10 system. It’s still new. It’s still growing and maturing. And it is becoming more complex as they add more specific codes. And then, there are the yearly changes that coders must keep up with in the official coding guidelines, as well as addition, deletion and changes in the actual ICD-10 codes. The in-patient accuracy rates that we’re currently experiencing are lower than expected and point to a need for improvement.
An example, Mike, is that according to the Central Learning System 2018 Coder Performance Data, the ICD-10 in-patient coding accuracy was 57% which is a little bit lower than the 2017 results that were 61%.
That brings us a fairly wide gap from the AHIMA’s ICD-9 benchmark of 95%.
Now, HIM professionals working in the trenches of coding and CDI may not be surprised by the lower coding accuracy results. However, other revenue stakeholders don’t always see a clear correlation between sub-optimal accuracy and reimbursement. This disconnect in coding accuracy expectations can sometimes be caused by multiple departments working in silos across the revenue cycle with blurred lines of responsibility and communication. This may be one of the biggest impacts in mid-revenue cycle vulnerability.
And sometimes, Mike, it’s a matter of raising awareness. In fact, during my recent webinar polling question, 58% of the audience did not know what their in-patient coding accuracy was.
Mike: Wow! Well, what can you tell us about clinical documentation improvement vulnerabilities?
Laura: Well Mike, if there’s a single word I would use to best describe how to improve physician clinical documentation, it would be specificity.
With seven times more codes than ICD-9, ICD-10 coding system can enable healthcare providers to enter much more specific data about an individual’s diagnosis and treatment. That is really what ICD-10 was designed for.
And armed with those specifics based on more detailed and precise coding, doctors and hospitals can monitor and manage disease patterns and provide better and more informed care across the patient continuum.
But with increased complexity in the coding and clinical documentation comes a need again to break down those silos between finance and clinical departments as well as silos between coding and CDI for ICD-10 to really reach its full potential. But due to the complexity of the mid-revenue cycle, this can be challenging.
The other thing, Mike, is the specificity needs change from year to year as data analysis uncovers new details on how information relates to the cost of patient care. One year, everyone reminded their doctors to specify whether the patient’s diabetes was insulin-dependent, and if there were any effects such as diabetic neuropathy. Now, the next year, they cared about whether the diabetes was controlled. Now, we want to know if it’s type 1 or 2, and if it’s controlled on admission. As a result, even specificity is a moving target.
Because all DRG’s are based primarily on what the physician documented, it’s financially critical to get complete information on the front-end of patient care.
Mike: Laura, what activities can a hospital engage in to minimize risk and safeguard revenue for the mid-revenue cycle inclusive of coding and clinical documentation?
Laura: Well Mike, coding and clinical documentation auditing is one process used to verify that physician documentation is complete and supports a claims code assignment and sequencing to arrive at the optimal DRG. Auditing can be conducted retrospectively or pre-bill. Many revenue cycle teams are opting to perform audits as quickly as possible to prevent claim denials.
By doing so, hospitals can receive greater benefit from their DRG and coding audit investments.
Mike: Laura, what about resources? We often hear that one barrier to auditing and other revenue integrity activities is just a lack of resources in a hospital. What can you tell us about that?
Laura: I do hear that too, Mike. But I really believe that the benefits of a comprehensive auditing program do far outweigh the costs. Claim rejections and claim denials are really creating a considerable financial burden for US hospitals and health systems. And despite new revenue cycle technology, managing all those denials remains a costly and time-consuming effort.
Many organizations, Mike, simply walk away, choosing not to correct, resubmit or appeal their results. Millions are rightfully provider dollars are left in the pockets of Medicare and third-party payers.
Certainly, I think a smarter strategy is to avoid those losses associated with denied in-patient claims by increasing the percentage of claims looked at in the first place. Investments in people, processes and technology to prevent these denials are far more effective than dollars we’re spending on managing them.
As hospitals and the health systems benefit from denial management over to denial prevention, in-patient coding and CDI audits have re-emerged lately as an effective reimbursement retention strategy.
The other piece is for hospitals to engage with the right revenue cycle partner. With the right partner, your organization can build a comprehensive program that improves coding and provider performance and addresses both compliance and revenue risk.
So Mike, although revenue integrity efforts do require resources, leveraging an external partner is one option that can lighten the load and the expense. The days of manual coding audits are behind us. And new technologies in place today allow hospitals to look at hundreds of claims and analyze them for improper payment in just a few minutes.
Those claims are then flagged for further review and can be looked at by an experienced coding analyst.
So, there are many benefits to including these audits, including timeliness, the volume of claim reviews, and also, a significant reduction in claim denials.
Mike: And Laura, we talked about several different resources here on the podcast today, a recent webinar, a body of research, a whitepaper. For members of our audience that would like to dig into those resources and look at them in detail, you can go to besler.com/insights. You’ll see a little tab that says revenue integrity. You can click on that and get access to all of those resources.
One other thing before we break for today, I’d just like to ask our audience—which is thousands of people each and every month, and we really appreciate that—if you do have any comments, questions about the podcast, ideas for topics that you’d like to hear about, I’d like to invite you to reach out to me personally at update@Besler.com. We would certainly love your feedback.
Laura, thank you so much for joining us on the podcast today and shedding some light on revenue cycle vulnerabilities.
Laura: You’re welcome Mike. Thank you.





